Comments:
Post-radiation Angiosarcomas: They make up about 25% of all angiosarcomas and are seen in the following clinical settings:
- In women who had lumpectomy followed by radiation for breast cancer (risk <1% of cases)
- In the abdominal wall/cavity following radiation for gynecologic cancers
- Following radiation for benign conditions (hemangiomas, tinea capitis) or other cancers
The
incidence of angiosarcoma in
previously irradiated breasts is estimated to be
0.16%. The location tends to
cutaneous, with very few cases involving the breast parenchyma itself. The latent period is around
5 years but may be as short as 3 years. This is shorter than latency at other locations, perhaps due to the large surface area of skin over the breast.
High doses of radiation are involved with a mean dosage of
50 Gy.
Clinical Features: The lesions are
large and multifocal and present as
bruise-like, indurated, ecchymotic or multinodular areas in a background of
radiation-damaged skin. Most patients come with complains of a
rash and the clinical appearance can
mimic infectious mastitis or
inflammatory breast carcinoma. There is
no associated lymphedema.
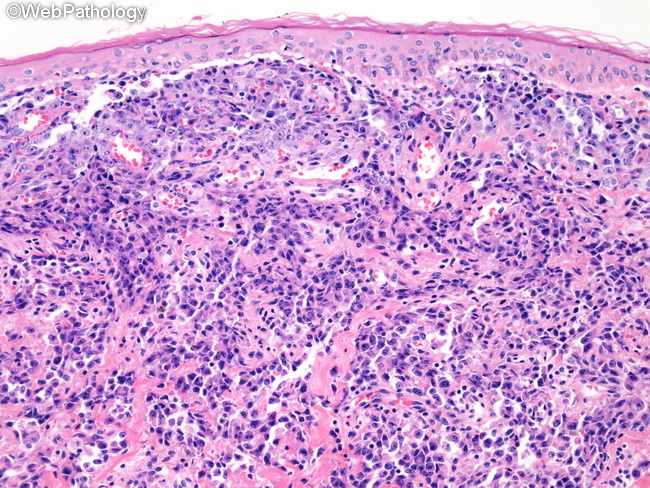
Case History (images 37-40): The patient was an
elderly female who underwent
lumpectomy, axillary lymph node dissection, and
radiation for
invasive ductal carcinoma of breast. She presented with a
breast mass 9 years later (same breast). An incisional biopsy was interpreted as poorly-differentiated recurrent invasive ductal carcinoma resulting in a mastectomy. The
mastectomy specimen showed
multiple reddish-purple macular areas on the skin and
hemorrhagic lesions in the subcutaneous tissues. The tumor was
poorly-differentiated with epithelioid morphology and located largely in the skin and subcutaneous tissues with focal invasion of breast parenchyma as well as chest wall structures. The peripheral portion of the tumor had more typical morphology of angiosarcoma consisting of
anatomosing vascular channels lined by
atypical endothelium (next three images). The tumor cells were
positive for
endothelial markers CD31, CD34, ERG, and claudin 5 and
Factor VIII-related antigen as well as
PROX1; they were
negative for EMA, CAM5.2, AE1/AE3, S-100, and HMB-45. There was
strong nuclear MYC immunoreactivity indicating
MYC gene amplification which is a feature of radiation-associated angiosarcomas. However, this feature may also be seen in other malignancies and is not specific for radiation-induced angiosarcomas.