Jan 2016
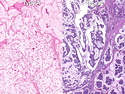
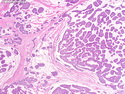
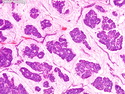
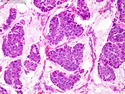
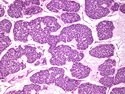
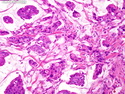
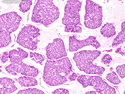
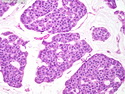
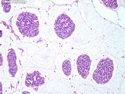
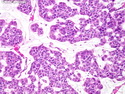
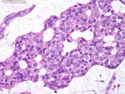
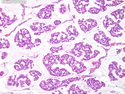
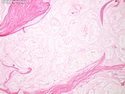
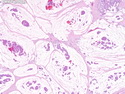
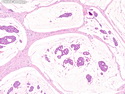
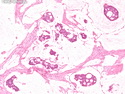
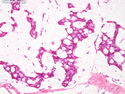
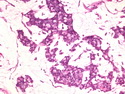
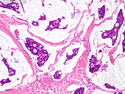
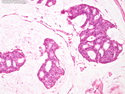
Mucinous (Colloid) Carcinoma
Reviewer(s): Dharam M. Ramnani, MD
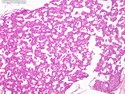
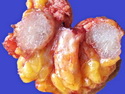
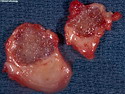
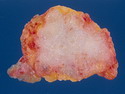
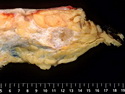
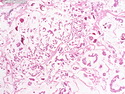
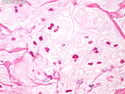
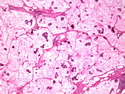
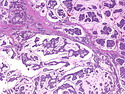
Pure mucinous (colloid) carcinoma makes up about 2% of all breast carcinomas. Focal mucin production is seen in additional 2% of breast cancers. The term mucinous carcinoma is restricted to the tumors showing stromal mucin in >90% of the tumor and excludes 1) mixed tumors containing areas of ordinary invasive ductal carcinoma, and 2) signet ring-cell carcinomas. The patients are usually post-menopausal. The tumors are well-circumscribed and have a gelatinous, bluish-gray cut surface. Microscopically, well-differentiated tumor cells arranged in solid nests, trabecular formations, cribriform clusters, or papillary structures are seen floating in pools of copious extracellular mucin.Immunohistochemical profile: Mucinous carcinoma shows strong cytoplasmic positivity for MUC2 and decreased MUC1 immunoreactivity when compared to ductal carcinoma. Hormone receptors ER and PR are always positive; HER2 is negative. Many cases express WT1. Between 25% to 50% of cases show neuroendocrine differentiation and are positive for NSE and related markers. Mucinous carcinomas – types A and B. Some authors have proposed subclassification into types A and B. Type A mucinous carcinomas are a distinct entity. Type B tumors show neuroendocrine differentiation. The short-term prognosis of mucinous carcinoma of breast is excellent. However, the tendency for delayed recurrences necessitates long-term follow-up. The incidence of nodal metastases is 2-4%. The presence of neuroendocrine differentiation does not appear to affect the prognosis.



.jpg)