Sezary Syndrome : Diagnosis

Comments:
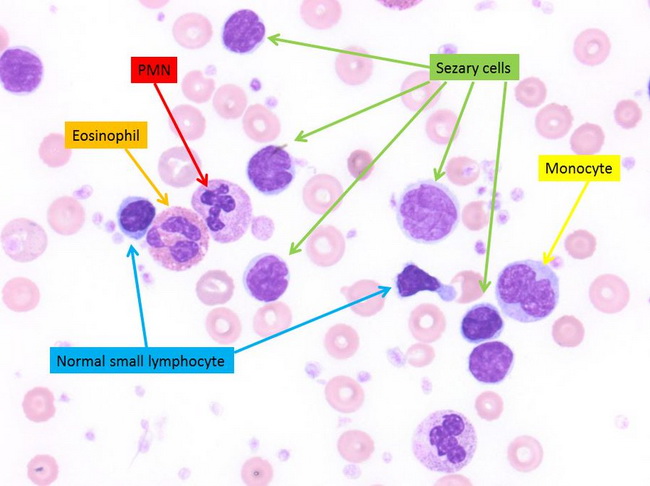
Sezary syndrome (SS) - Diagnosis: The diagnosis of SS previously relied on the presence of Sezary cells (neoplastic T-cells with hyperconvoluted, cerebriform nuclei) in the peripheral blood. However, this finding is not specific as circulating Sezary cells may be found in normal individuals and in benign conditions. The current diagnostic criteria proposed by ISCL* and adopted by the WHO/EORTC* integrate clinical, histopathologic, immunophenotypic and molecular findings. In a patient with erythroderma, the diagnostic criteria for Sezary Syndrome include:
- Absolute Sezary cell count of ≥ 1000 cells/μL. The presence of large Sezary cells (>14 μm in diameter) is a more specific but less sensitive finding. Small and intermediate Sezary cells may be seen in benign conditions, including contact dermatitis, atopic dermatitis, erythrodermic psoriasis, eczema, actinic reticuloid, drug reactions, and as an incidental finding in the blood of healthy elderly people.
- Flow cytometry showing expanded CD4+ cell population resulting in CD4/CD8 ratio of ≥10:1
- Aberrant loss of pan-T-cell markers, including CD2, CD3, CD4, CD5, CD7, and/or CD26 by flow cytometry
- Loss of CD7 in ≥40% of lymphocytes, OR loss of CD26 in ≥80% of lymphocytes.
- Demonstration of the same abnormal T-cell clone in both peripheral blood and skin with TCR gene rearrangements. Abnormal T-cell clones in the peripheral blood by PCR or Southern blot may rarely be seen in benign conditions and as an incidental finding in the elderly, When the same abnormal clone is identified in other locations such as skin or lymph node, it is more clinically meaningful.
- Chromosomally abnormal T-cell clone



