Mycosis Fungoides : Differential Diagnosis

Comments:
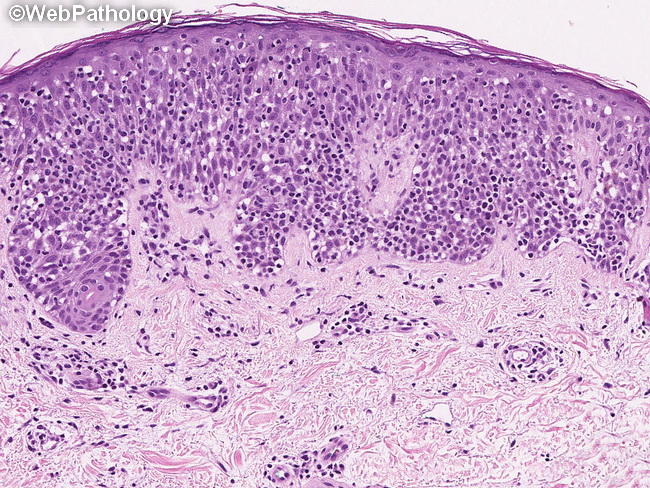
Mycosis fungoides (MF) - Differential Diagnosis of Patch Stage: The correct diagnosis of MF in early lesions of patch stage can be quite challenging. It resembles a large number of inflammatory skin conditions clinically and pathologically. The microscopic findings in early stages are subtle and easily missed. If MF is suspected clinically, it may require several biopsies to make the diagnosis with confidence. The median time from symptom onset to diagnosis is 3 to 4 years, but it may exceed decades. The lymphocytic infiltrate contains few or no atypical cells and can mimic other inflammatory dermatoses. The recognition of MF is based more on identifying the pattern of infiltration rather than the presence of atypical cells with cerebriform nuclei. Patch Stage: The differential diagnosis includes - eczema, psoriasis, large-plaque parapsoriasis, poikiloderma, psoriasiform lichenoid dermatitis (lichen striatus, lichen sclerosus et atrophicus, persistent pigmented purpuric dermatitis), spongiotic dermatitis (allergic contact or nummular dermatitis), and interface dermatitis (lichenoid drug eruptions, lichenoid keratoses). MF should be considered in patients with "atypical" or "refractory psoriasis." Plaque and Tumor Stages: The differential diagnosis includes other T-cell lymphomas, including peripheral T-cell lymphoma, NOS, anaplastic large cell lymphoma, and CD4+ small/medium-sized T-cell lymphoma. Clinical presentation is the key in differentiating these conditions from MF as the histologic picture may be similar. This image shows striking epidermotropism. Numerous atypical lymphoid cells are scattered throughout all the layers of epidermis.



