Pulmonary MALT Lymphoma : Differential

Comments:
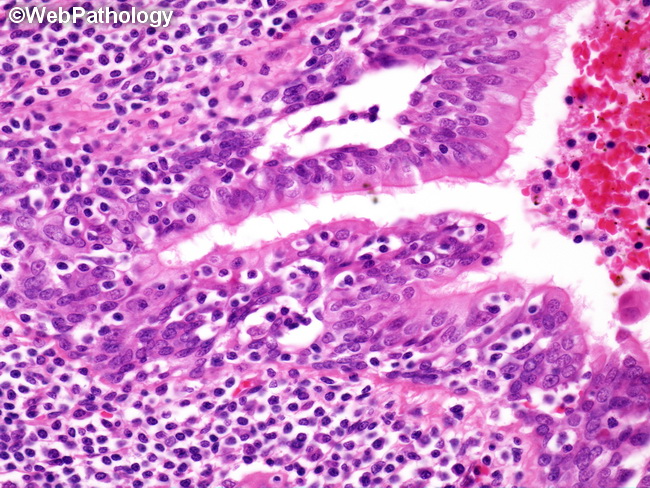
The differential diagnosis of pulmonary MALT lymphomas includes reactive lymphoid proliferations such as nodular lymphoid hyperplasia and lymphocytic interstitial pneumonia as well as other B-cell lymphomas. Features favoring pulmonary MALT lymphomas include: poorly circumscribed mass lesion with peripheral spread in a lymphangitic pattern along alveolar walls, predominance of B cells with features of marginal zone cells, plasma cells/plasmacytoid cells with light chain restriction, aberrant expression of CD43 on B cells, and demonstrating a monotypic B-cell population with flow cytometry or genetic studies (clonal Ig gene rearrangements, MALT1-associated translocations). Features favoring Nodular Lymphoid Hyperplasia: well-circumscribed solitary peripheral lesion (rare cases have multiple lesions), lack of peripheral lymphangitic spread, lymphoepithelial lesions rare or absent, no infiltration of pleura, no evidence of clonality by molecular studies, lack of light chain restriction by plasma cells, and reactive follicles with typical distribution of B- and T-cells. Lymphocytic interstitial pneumonia is a diffuse interstitial lung disease generally seen in patients with underlying collagen vascular disease or immunodeficiency. Imaging studies show bilateral diffuse ground glass opacities. Morphologically, the lymphocytic infiltrate is confined to the interstitium and expands the alveolar septa. Architectural effacement with formation of a mass is not seen in LIP. Immunohistochemical stains and molecular studies show a polyclonal process. The image shows prominent infiltration of the bronchiolar epithelium by neoplastic lymphocytes creating lymphoepithelial lesions. This is accompanied by degenerative changes in the epithelium.



