MALT Lymphoma : Pathogenesis

Comments:
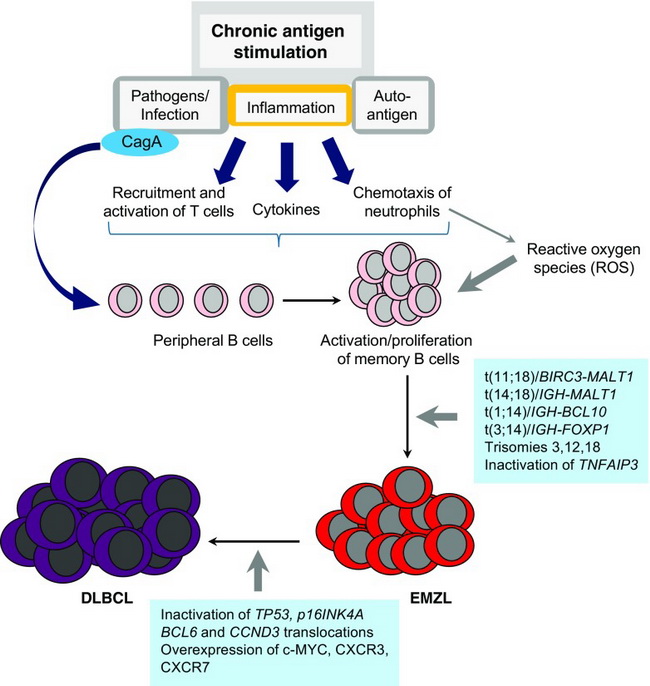
MALT Lymphoma - Pathogenesis: Extranodal marginal zone lymphomas (EMZL) usually arise in acquired mucosa-associated lymphoid tissue (MALT) in the setting of chronic inflammation of bacterial, viral, autoimmune, or unknown etiology. They begin as a polyclonal immune response to an antigen (e.g. Helicobacter pylori or an autoantigen (e.g. Sjogren syndrome) which eventually leads to the emergence of a B-cell clone. At this stage, the clonal neoplastic lymphocytes are still dependent on antigen-stimulated helper T-cells for growth and survival. Eradicating the antigenic stimulus, e.g. with antibiotic or antiviral therapy, can cause tumor regression. If the antigenic stimulus persists, the lymphoma cells acquire additional genetic alterations which make them antigen-independent for growth and survival. These alterations include t(11;18), t(14;18), t(3;14) or t(1;14) chromosomal translocations which upregulate BCL10 or MALT1 expression. This causes constitutive activation of NF-κB signaling pathway that promotes B-cell survival and growth. With accumulation of additional genetic lesions, some cases transform to diffuse large B-cell lymphomas (DLBCL). Translocation-negative cases of EMZL show mutation or deletion of chromosome 6q23 involving TNFAIP3 (A20) which is a negative regulator of NF-κB pathway. Image source: Schreuder MI et al. Novel developments in the pathogenesis and diagnosis of extranodal marginal zone lymphoma. J Hematop. 2017 Dec. 10(3-4): 91-107. Used under Creative Commons Attribution 4.0 International License.



