Endometrial Hyperplasia : Diagnosis

Comments:
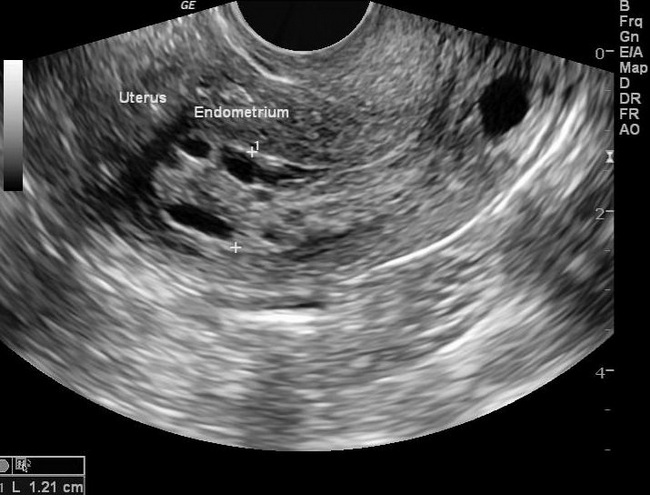
Diagnosis of Endometrial Hyperplasia (EH): EH is typically diagnosed on endometrial biopsy or curettage performed in women who present with postmenopausal bleeding. About 15% of women with postmenopausal bleeding are found to have EH on sampling. EH may be picked up incidentally (as thickened endometrium) on transvaginal ultrasound during work-up for infertility, abdominal pain, or other complaints. Postmenopausal women with a thickened endometrial lining (>5 mm) or women with persistent unexplained vaginal bleeding should undergo endometrial biopsy. Rarely, atypical glandular cells show up on a Pap smear, prompting an endometrial biopsy. In such situations, almost one-third of patients are found to have clinically significant uterine pathology requiring intervention. The risk of finding adverse pathology is especially higher for women above 50 years of age. Women below 40 years of age with abnormal uterine bleeding who have risk factors for endometrial carcinoma such as obesity or polycystic ovarian syndrome should be evaluated comprehensively. Endometrial ultrasound and, in some cases, endometrial biopsy/curettage may be required. Case History: 65 y/o female with post-menopausal bleeding. Ultrasonography of the uterus showed endometrial thickness of 12 mm. Multiple cystic spaces were noted. The patient underwent endometrial biopsy which showed nonatypical EH. Transvaginal ultrasound for measurement of endometrial thickness is a useful noninvasive technique for initial assessment of women with irregular or postmenopausal bleeding. In a symptomatic postmenopausal patient, endometrial thickness > 5 mm is considered abnormal. However, thickened endometrium on ultrasonography is a non-specific finding and requires histopathologic examination for the diagnosis of EH. Case courtesy of Dr Maulik S Patel, Radiopaedia.org. From the case rID: 30100



